Premenstrual dysphoric disorder (PMDD): when PMS becomes a challenge
Author: Dr. med. univ. Martin Kiebler
Hello there! My name is Martin and I’m excited to welcome you to this blog article series about Premenstrual Disorders (PMD).
In our previous blog article, we covered the topic of premenstrual syndrome (PMS). We talked about how to diagnose PMS, what potential symptoms can occur, and how to treat it. However, in this blog post, we'd like to focus on a more specific and intense form of premenstrual syndrome known as premenstrual dysphoric disorder (PMDD). We will explore PMDD in depth, including its causes, symptoms, and treatment options, to help you better understand this condition and seek medical help if necessary.
What is premenstrual dysphoric disorder (PMDD)?
PMDD is a hormonal disorder that occurs in some women in the days leading up to their period. The reason for this is thought to be an imbalance/abnormal interaction of sex hormones and neurotransmitters in the brain and may be in part as well genetically determined (check out this blog post to read more about this!).
Unlike PMS, which causes mild to moderate symptoms in many women, PMDD is characterized by more severe emotional, psychological, and physical symptoms, that significantly limit daily life. Over the duration of their reproductive years, women with PMDD are thought to be disabled for an average of 3.8 years!
Symptoms
Symptoms of PMDD may differ among women but typically occur in the days before their period and subside shortly after menstruation begins.
While PMS is common and affects up to 75% of menstruating women, PMDD is a more severe and less frequent form of PMS that significantly impacts a woman's mental health and overall well-being.
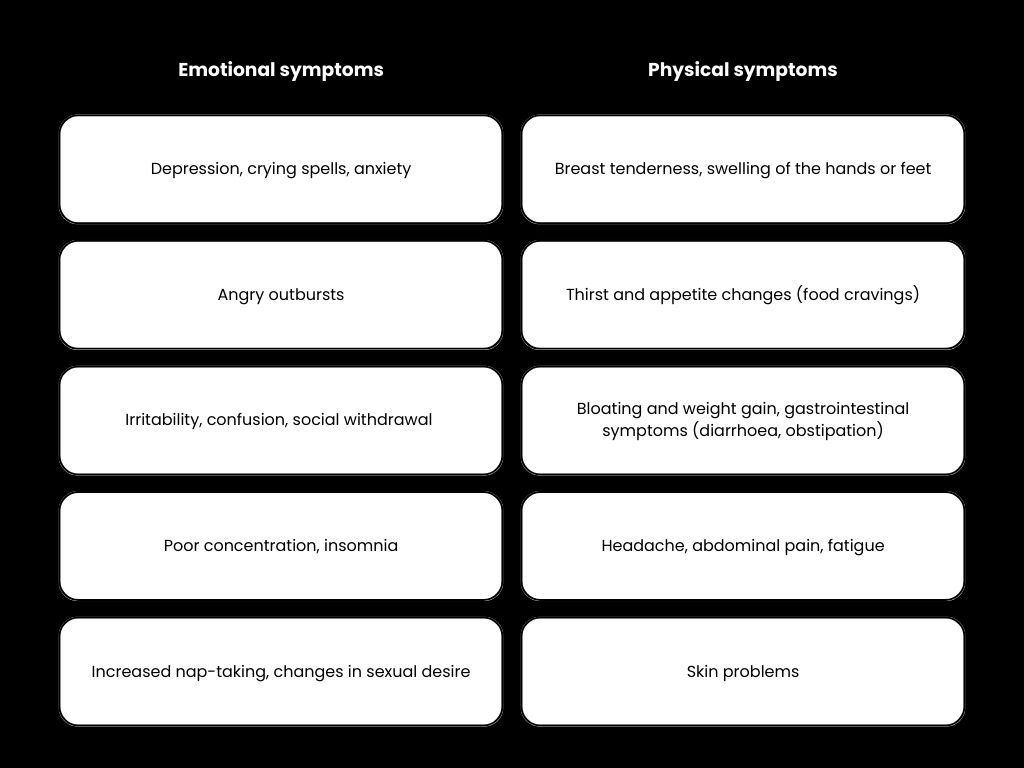
The most common symptoms are:
Extreme mood swings: women with PMDD experience intense mood changes, which can range from abrupt outbursts of rage and impatience to depression and hopeless feelings.
Anxiety and feelings of tension: PMDD may also be accompanied by severe anxiety and general tension.
Depressed mood: women with PMDD may experience depressive symptoms during this time, such as sadness, dejection, and loss of interest.
Irritability and anger: often, women suffer from intense irritability and outbursts of anger, which may lead to tensions in their relationships.
Physical symptoms: in addition to emotional and psychological symptoms, affected women may also experience the same physical symptoms as with PMS such as breast tenderness, headaches, fatigue, and muscle pain.
Diagnosis
Diagnosing PMDD can be challenging because symptoms can be mistaken for other conditions such as depression or anxiety disorders. Women suffering from PMDD need to discuss their symptoms with a healthcare professional. Taking a closer look at the menstrual cycle and symptoms can help make an accurate diagnosis.
Just as with PMS, keeping a diary of symptoms makes sense to document the temporal context within the menstrual cycle. This helps with diagnosing PMDD.
There are no customized laboratory tests that can identify PMDD, but they can be done to filter out other possible causes of similar symptoms such as thyroid disorders or other organic diseases. A thorough medical anamnesis that includes a detailed discussion of symptoms, menstrual cycle, and impact on daily life is critical to making the diagnosis.
The diagnosis of PMDD is based on predefined criteria found in the so-called DSM-5 system. To be diagnosed with PMDD, you must experience at least five of the following symptoms during the week before your period, for at least two consecutive menstrual cycles:
You may be asking, “What if I use an IUD or have had uterine surgery and no longer get my period, but I still experience the symptoms listed above?” Keeping a PMS diary to track the symptoms' cyclical pattern is crucial in this situation.
If you are experiencing any of these symptoms, speaking with your gynaecologist about getting a proper diagnosis and treatment plan is important. Additionally, according to the DSM-5 criteria, PMDD may coexist with other psychiatric conditions (e.g., depression) as long as it does not merely worsen them. Premenstrual disorders should always be distinguished from an underlying major psychiatric disorder, menopausal transition, thyroid disorders such as hyper- or hypothyroidism, or endometriosis before diagnosing PMDD.
Therapy
The treatment goal for PMDD aims to reduce symptoms and improve the quality of life of those affected. Depending on the severity of the symptoms and your needs, a variety of methods can be considered.
Common treatment options include:
1. Drug therapy: antidepressants, especially selective serotonin reuptake inhibitors (SSRIs), are often used to treat PMDD. These drugs work by increasing the levels of serotonin in the brain, which can help regulate mood swings and reduce symptoms of depression and anxiety. These medications must be used under a doctor's supervision because they can have side effects such as nausea, headache, and decreased libido. Previously, a drug called alprazolam (benzodiazepine) was used specifically to reduce PMDD symptoms. However, this drug is no longer recommended by international guidelines.
2. Hormonal therapy: for some women, taking hormonal contraceptives, such as combination pills (combined oral contraceptives = COC) that regulate the menstrual cycle, may help relieve symptoms of PMDD. However, this approach should be discussed with a physician, taking into account individual risk factors.
3. Cognitive behavioural therapy (CBT): CBT support may be helpful to develop coping strategies and help manage the symptoms of PMD if a suboptimal response to pharmacologic treatment is observed. It can be particularly effective in managing negative thinking patterns and applying stress management techniques.
4. Lifestyle changes: Certain lifestyle changes can help relieve symptoms. These include regular exercise, getting enough sleep, stress reduction techniques such as relaxation and meditation, eating a balanced diet, and avoiding alcohol and caffeine.
CONCLUSION
PMDD is a serious condition that can significantly impact women's lives. It is important to discuss symptoms with a medical expert to get an accurate diagnosis and receive the best possible treatment. With the right diagnosis and a holistic approach to treatment, the symptoms of PMDD can be effectively relieved and quality of life improved.
This article was written by our guest author Martin as part of his series about Pre-Menstrual-Disorders.
Sources & further reading: