Cracking the premenstrual code: understanding what causes PMS and PMDD
Author: Dr. med. univ. Martin Kiebler
Ah, the mysterious world of hormones. These tiny chemical messengers can majorly impact women's bodies and minds, leaving them feeling like they’re on a rollercoaster ride of emotions. The last three blog posts within the PMD blog series addressed the two main actors of premenstrual disorders – Premenstrual Syndrome (PMS) & Premenstrual Dysphoric Disorder (PMDD), as well as some promising therapeutic options for them.
Have you ever wondered what's happening inside the body during this tumultuous time? Come and explore with us as we delve into the mechanisms that contribute to the development of PMS and PMDD, gaining a deeper understanding of how our body functions and interacts.
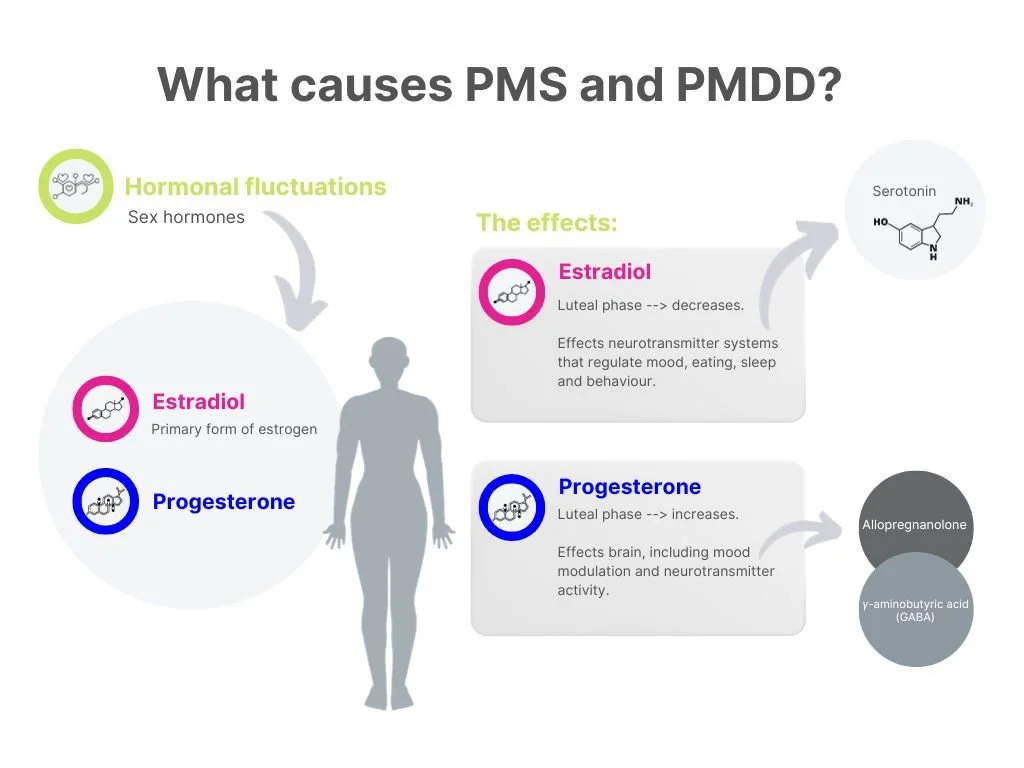
KEY PLAYERS: PROGESTERONE and ESTRADIOL
Before we dive into the depths of PMS and PMDD, let's first meet the key players: progesterone and estradiol. Progesterone and estradiol are two sex hormones that play crucial roles in the menstrual cycle.
Progesterone's Role and Effects
Progesterone, often referred to as the "pregnancy hormone," is vital in preparing the body for conception and supporting a potential pregnancy. This hormone is produced by the ovaries following ovulation. Its primary function is to prepare the uterine lining (endometrium) to receive a fertilized egg. If fertilization occurs, progesterone helps maintain the pregnancy by supporting the growth and development of the embryo.
However, progesterone is not solely involved in reproduction. It also exerts various effects on the brain, including modulating mood and neurotransmitter activity. During the menstrual cycle, progesterone levels rise in the second half of the cycle to prepare the body for pregnancy. If conception doesn't occur, progesterone levels drop, leading to the shedding of the uterine lining and the onset of menstruation.
Estradiol's Role and Effects
Estradiol, the primary form of estrogen in the female body, is a multifaceted hormone with an array of responsibilities. Produced mainly by the ovaries, estradiol is involved in the growth and development of female reproductive organs, breast tissue, and the menstrual cycle regulation. It promotes the proliferation of the uterine lining and supports the maturation of eggs within the ovaries. Throughout the menstrual cycle, estradiol levels fluctuate, peaking just before (and there through leading to) ovulation and declining thereafter. These fluctuations can contribute to the emotional and physical changes experienced during the premenstrual phase.
Hormonal fluctuations
As the menstrual cycle progresses, the levels of progesterone and estradiol fluctuate (see Figure 1 below). These hormonal ups and downs set the stage for PMS and PMDD symptoms. Symptoms of PMS start at the time of ovulation and increase with the rise of sex hormones. Interestingly, it's not the absolute levels of these hormones that cause trouble, but rather the changes and fluctuations that accompany their rise and fall. Once hormone levels return to those seen in the follicular phase (about two weeks before ovulation), the symptoms disappear. This suggests that hormonal fluctuations and the body's accompanying enhanced responsiveness, rather than increased hormone levels themselves, play a key role in PMS/PMDD. Another hypothesis suggests that the enhanced sensitivity to fluctuating hormone levels in PMS and PMDD is influenced by multiple factors, some of which may be genetically determined. Studies have shown genetic variations in estrogen and serotonin receptors in women with PMS/PMDD, which could affect how fluctuating estrogen levels during the luteal phase impact PMS symptoms, potentially leading to cell-signaling problems.
ALLOPREGNANOLONE and GABA in PMS/PMDD
Progesterone quickly changes into other substances in the brain, like allopregnanolone (ALLO) and pregnanolone. One hypothesis is that ALLO interacts with receptors in the brain, affecting the activity of γ-aminobutyric acid (GABA), a key chemical that helps calm the central nervous system. Normally, GABA has relaxing and calming effects. However, when ALLO binds to GABA receptors, it prevents GABA from working properly. ALLO itself has a calming effect, but in patients with PMS/PMDD, it's thought that the receptors might become less responsive, causing the opposite effect and leading to symptoms like feeling anxious and irritable.
THE EMOTIONAL ALCHEMIST
Another key player regarding PMS and PMDD is serotonin, a neurotransmitter significantly impacting mood regulation. Studies have shown that serotonin levels may be reduced during the luteal phase, contributing to dysphoric symptoms experienced by individuals with PMS/PMDD. Medications that increase serotonin levels, such as selective serotonin reuptake inhibitors (SSRIs), have been found to alleviate these symptoms, further supporting the link between serotonin and PMS/PMDD.
DECODING ESTRADIOLS IMPACT
Estradiol, as mentioned earlier, is involved in the menstrual cycle and has multiple effects on neurotransmitter systems that regulate mood, eating, sleep, and behavior. In women with PMDD, estradiol is believed to increase serotonin transporters, particularly in brain areas involved in emotion and behavior. This leads to increased transport of serotonin into cells, limiting its ability to act as a neurotransmitter. This can potentially be observed through low serotonin levels in blood samples during the luteal phase.
STRESS vs. ALLO
The relationship between the development of PMS/PMDD and a history of significant stress exposure is still unclear and is an area of ongoing research. While some studies have found an association between trauma history and PMDD diagnosis, others have not found any connection. One potential mechanism involves the interaction between stress and allopregnanolone. While ALLO levels typically increase in response to stress, women with PMS/PMDD do not show this typical increase. Animal models have shown that repeated, chronic stress can reduce ALLO levels, leading to a lack of stress regulation without compensatory mechanisms.
BREAKTHROUGHS for PMS/PMDD
Modifying the formation of neurotransmitters and neuroactive steroids, such as ALLO, that impact the GABAergic system may hold the key to developing effective drugs against PMS/PMDD. However, more scientific work and larger studies are needed to comprehensively understand the pathophysiology.
Conclusion
The pathophysiology of PMS and PMDD is a fascinating interplay of hormonal fluctuations, neurotransmitter imbalances, genetic variations, and brain activity. While the journey to fully comprehend these conditions is ongoing, it is essential to remember that support is available. If you find yourself dealing with symptoms of PMS or PMDD, reach out to your gynecologist for further guidance and support.
Be sure to check out theblood’s Hey Period shake that is a protein shake enriched with supplements known to help reduce and alleviate PMS symptoms.
CLICK HERE to find out more!
This post is part of our PMD blog series by Dr. med. univ. Martin Kiebler.
References: