Revolutionizing Menstrual Product Testing: A Breakthrough for Heavy Bleeders
Discovering How Well Menstrual Products Actually Work: Testing with “Real” Blood
In 2023, a significant stride has been made in the realm of menstrual product research. While it might sound surprising, until recently, menstrual products had never been properly tested with anything resembling real menstrual blood. But thanks to a recent study by DeLoughery et al. at the Oregon Health & Science University, the efficacy of various menstrual products has finally been assessed using human packed red blood cells.
In this article, we'll dive into the details of this study and explore its implications, particularly for those dealing with heavy menstrual bleeding (HMB).
Unmasking the True Capacity of Menstrual Products
Before we start, please just take a moment to think about menstrual blood. Can you agree that it is a unique bodily fluid, right? It doesn’t quite resemble water or even systemic blood that we see from cuts… does it? Menstrual blood for one, is not just blood. It is a complex bodily fluid composed of blood, cervical and vaginal secretions, endometrial tissue and cells, bacteria and more. It can be sticky and slimy, and even clumpy because of blood clots. And, there is no standard “type” of menstrual blood. Menstrual blood can differ from one day of menstruation to the next, from one person to another, and even look completely different altogether in another menstrual cycle of the same person. The point is, menstrual blood is unique [and this is what we love about it, but that’s another story you can read about HERE].
Unlike traditional testing of menstrual products, which involves using a saline solution as a substitute, in this new study, the researchers embraced a more accurate approach with something that is just a bit more comparable to menstrual blood. They utilized human packed red blood cells to mimic just some of the qualities of actual menstrual blood (the red blood cells at least). The outcome? Well, we now have a much clearer picture of how well menstrual products absorb or contain blood cells; something we didn’t know before apparently.
The Study
In the study, the researchers used laboratory testing to look at the maximum capacity of various commercially available menstrual products to both absorb and fill a solution containing red blood cells, where expired human packed red blood cells were used. Some of the menstrual products tested included tampons, sanitary pads (super/regular), menstrual cups, menstrual discs and period underwear, with 21 different types being analysed in total.
For each menstrual product, the volume of the red blood cell solution was recorded that was needed to saturate or fill the product. The results of the study showed that menstrual discs had the highest capacity, with an average of 61 ml being held. On the other hand, period underwear had the lowest capacity with 2 mL. For tampons and sanitary pads, 20-50 mL was shown to be needed to fully saturate the product, depending on the type being tested e.g. super/regular.
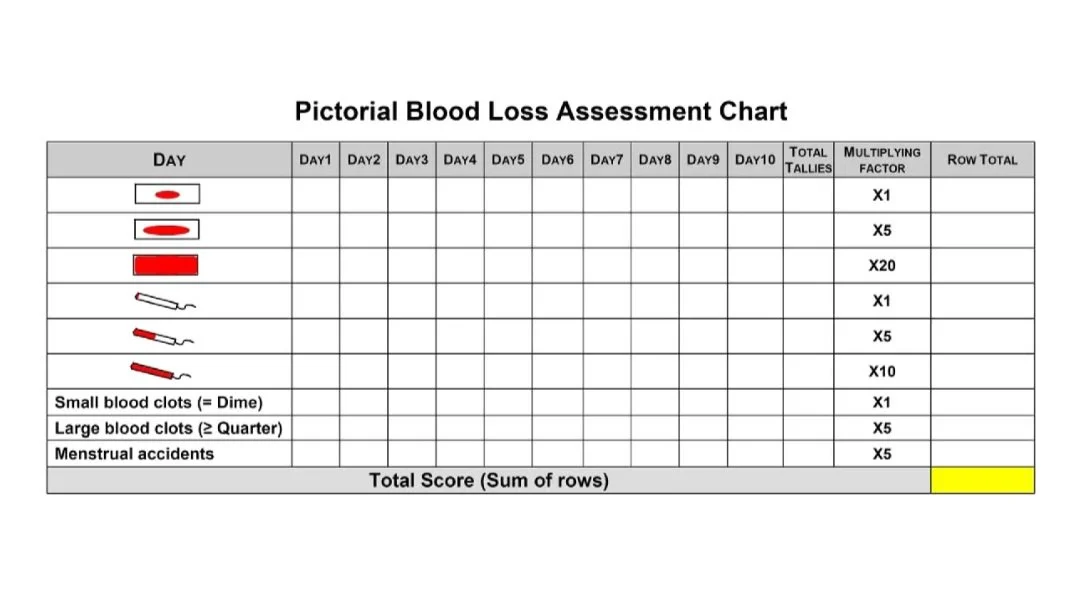
The Significance of The Study and Proper Menstrual Product Testing
Why is this research so crucial, especially for individuals with heavy menstrual bleeding? Well, firstly HMB affects approximately one-third of menstruating individuals. Heavy menstrual bleeding, often referred to as menorrhagia, is characterized by abnormally heavy and prolonged menstrual periods; losing more than 80 mL of menstrual blood per menstrual cycle. This condition can lead to considerable physical discomfort, emotional distress, and even anaemia through the loss of iron. Currently, clinicians rely on the Pictorial Blood Loss Assessment Chart (PBAC) to evaluate menstrual blood loss, primarily based on the saturation of tampons and pads (see image below). The PBAC method defines those with HMB or requiring medical attention due to extensive blood loss, as individuals needing to change a saturated pad or tampon every one to two hours. However, this assessment method falls short when it comes to accurately evaluating the capacity of menstrual products for managing real menstrual blood… as highlighted by the study.
The Pictorial Blood Loss Assessment chart [Reproduced from El-Nashar et al. 2015].
The Pictorial Blood Loss Assessment Chart (PBAC) is a semi-quantitative tool designed to evaluate menstrual blood loss by healthcare professionals. Patients are directed to look at their sanitary pad or tampon, prior to throwing it away after use, and to mark which one it looked like on the left column, mark how many small or large blood clots they observed, and whether they experienced a menstrual accident. This is completed for each day of menstruation, and then the tally is totalled to show the number for each throughout the entire menstrual cycle. With each one having a score relating to their meaning in terms of menstrual blood loss, a total score for the menstrual cycle can be calculated. The higher the score, the more menstrual blood is estimated to be lost during one menstrual cycle.
Challenging the Status Quo
The revelation from DeLoughery's study is twofold. Firstly, it provides valuable insights into the actual absorptive capacity of various menstrual products—ranging from menstrual cups and discs to specialized underwear. Not only were the capacities of sanitary pads and tampons shown to be different to what we believed before, based on saline solution testing, but now also more modern, and increasingly popular menstrual products have been tested, that could help modernise HMB diagnosis procedures. Secondly, it raises questions about the efficacy of the PBAC method. By comparing the capacity shown by manufacturers, often based on saline solution testing, to the real-world absorbency demonstrated with human packed red blood cells, the study sheds light on the potential underestimation of menstrual blood loss.
A New Era for Menstrual Health Evaluation
The implications of this research are far-reaching. For starters, we now possess a more accurate understanding of how well menstrual products can manage heavy flow. This information empowers individuals to make more informed choices about the products they use during their menstrual cycle. Additionally, the study urges a re-evaluation of the PBAC assessment, which could lead to better diagnosis and management of HMB. Misdiagnosis and the resulting health complications may be avoided by adopting a more precise approach to assessing blood loss.
Delving Deeper: Get the Full Story
If you're eager to delve into the nitty-gritty of the study, you can find the full article as a PDF in BMJ Sexual & Reproductive Health HERE.
Conclusion: Empowering Choices with Accurate Knowledge
The era of menstruation deserves an informed and scientific approach, and DeLoughery's study is a pivotal step in that direction. By embracing accurate testing methods, we're better equipped to navigate the unique challenges posed by heavy menstrual bleeding. With a clearer understanding of menstrual product efficacy, we can make choices that align with our individual needs and experiences. Those who struggle with heavy menstrual bleeding, are able to choose their menstrual products with more confidence, and medical professionals will be hopefully be able to diagnose HMB with more confidence too!
Overall, this study is a giant leap in terms of revolutionising HMB diagnosis and management, but also for menstrual health in general. It’s just a shame that it has taken until 2023 for researchers to actually do such a study (as many people on social media are pointing out…). This is, unfortunately, an effect of the Gender Health Gap and why it is now more important than ever for more studies like this one to be conducted, so we can advance menstrual health and women’s health, so that women actually get the healthcare and treatment they actually deserve.
References:
Further Reading: